Sweet Relief: Conquering Endodontic Pain Post-Treatment
Why Endodontic Pain Relief Matters to Your Comfort and Recovery

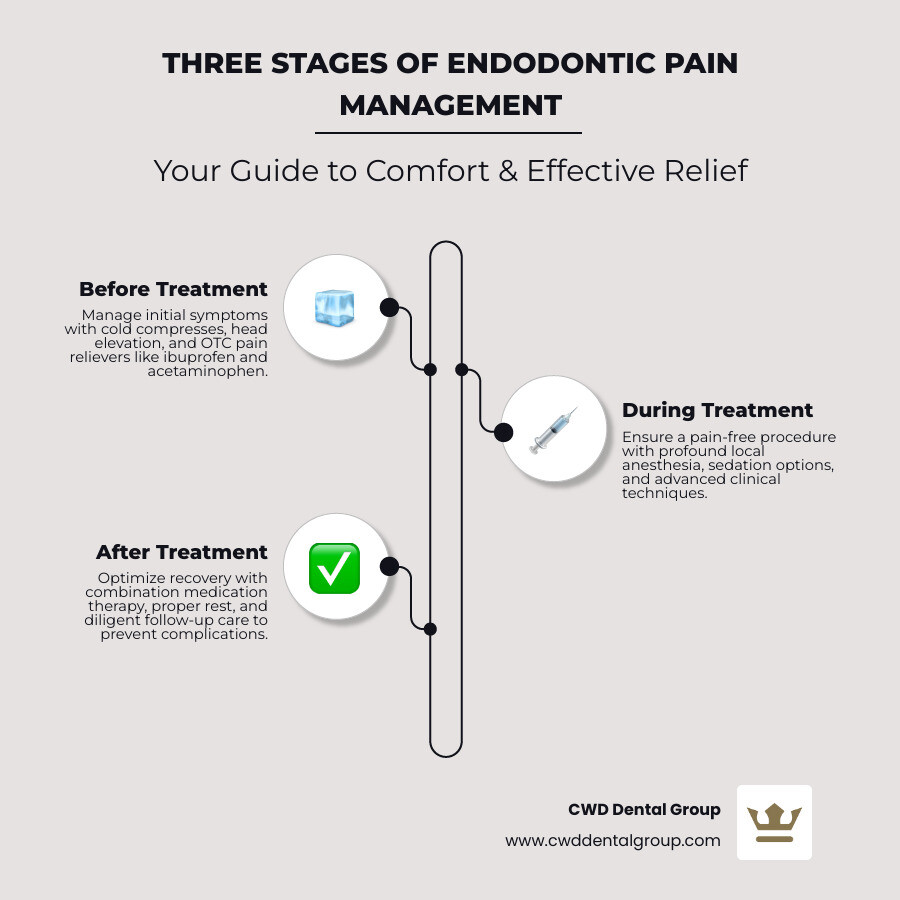
Endodontic pain relief is achievable through a combination of professional treatment, proper medications, and simple at-home care. Here's what works best:
Quick Relief Strategies:
- Over-the-counter pain relief: Combination of ibuprofen (400-600mg) and acetaminophen provides superior pain control
- Cold compress: Apply for 15 minutes on, 15 minutes off to reduce swelling
- Professional intervention: Root canal treatment removes the source of pain, not causes it
- Post-treatment care: Most discomfort resolves within 24-72 hours with proper medication
When to Seek Immediate Care:
- Fever or excessive swelling
- Unbearable pain not controlled by medication
- Signs of spreading infection
If you've just had a root canal or are preparing for one, you're likely wondering about pain management. The good news? Modern endodontic procedures are designed to eliminate pain, not cause it. Research shows that approximately 1.4% to 1.6% of cases result in significant post-treatment pain, and advances in anesthesia and technique have made the procedure itself virtually painless for most patients.
The reality is that the pain you feel before treatment is typically far worse than any discomfort afterward. Studies indicate that patients who received proper local anesthesia (confirmed by cold testing, not just a "numb lip") were approximately 80% less likely to experience pain during the procedure. Post-treatment, a combination of ibuprofen and acetaminophen has proven more effective than opioid medications, offering relief by targeting pain through both peripheral and central nervous system pathways.
I'm Kayle Vernon, and while my primary expertise lies in marketing and business growth, I've spent years helping healthcare practices like CWD Dental Group communicate complex medical information—including endodontic pain relief—to patients in clear, accessible ways. Through this work, I've gained deep insight into what patients need to know to feel confident and comfortable during their dental care journey.
Understanding the Root Causes of Endodontic Pain
When you experience dental pain, it's our body's way of telling us something is amiss. In endodontics, the pain often stems from issues deep within your tooth, specifically involving the dental pulp. This delicate tissue, nestled at the core of your tooth, contains nerves, blood vessels, and connective tissue. When it becomes inflamed or infected, pain can range from a dull throb to an excruciating agony.
The primary culprits behind this discomfort are usually pulp inflammation (pulpitis) and bacterial infection. Untreated cavities, cracks, or trauma can allow bacteria to invade the pulp, leading to an inflammatory response. This inflammation increases intrapulpal pressure, activating the sensitive nerve endings and causing the pain you feel. If left unchecked, this can lead to an abscess, a pocket of pus that forms at the tip of the tooth's root. This creates further pressure buildup, intensifying the pain and potentially spreading the infection. Symptomatic apical periodontitis, an inflammation of the tissues around the root, is also a significant predictor of severe postoperative pain.
We understand that knowing what's causing your discomfort is the first step toward finding endodontic pain relief. That's why we emphasize thorough diagnostic services to pinpoint the exact issue. More info about our diagnostic services
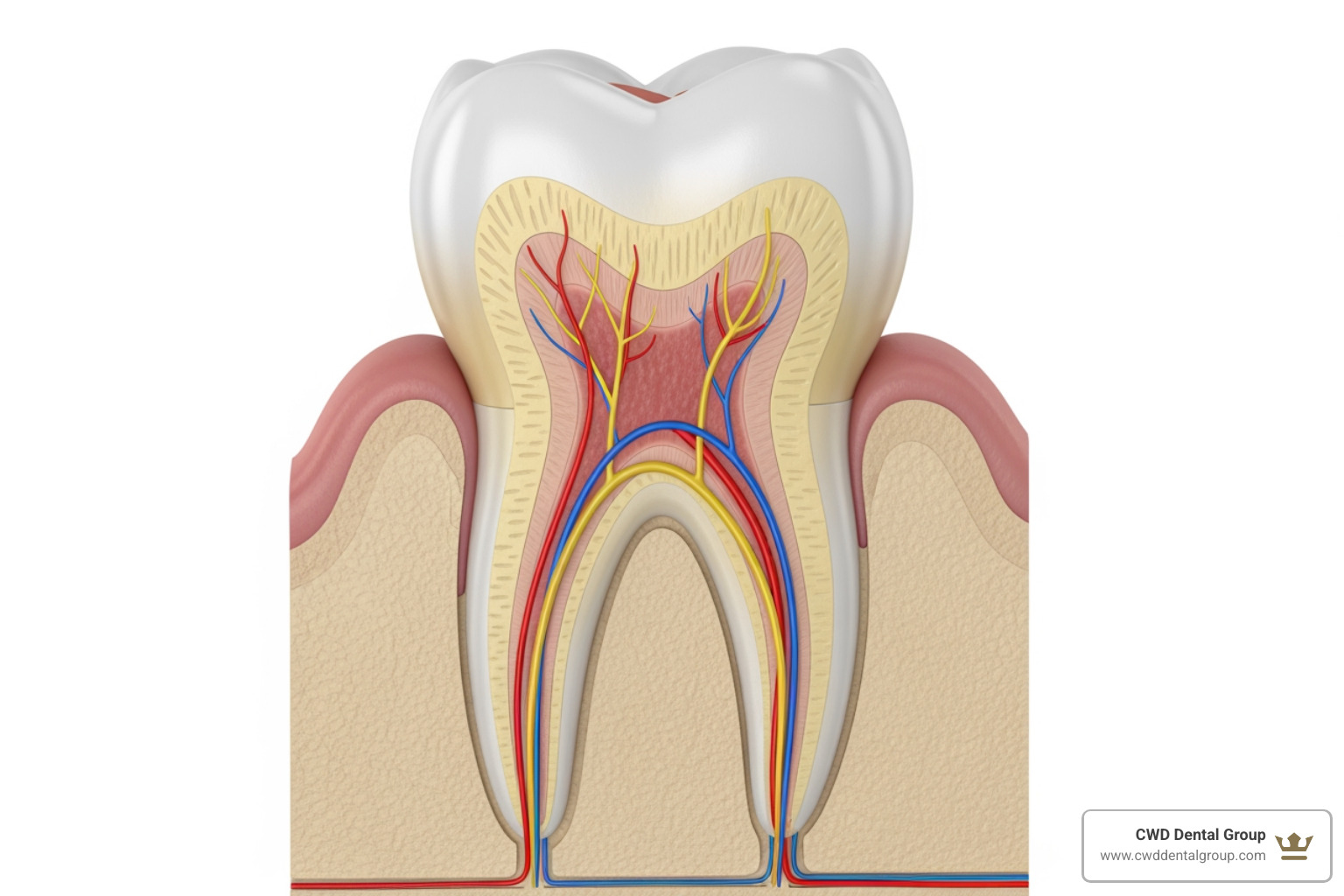
Why Does My Tooth Hurt So Much?
The intensity of tooth pain is largely due to the intricate network of nerves within the dental pulp. Two main types of nerve fibers, A-delta and C-type, are responsible for transmitting pain signals. A-delta fibers are myelinated and transmit sharp, sudden pain, often in response to cold stimuli. C-type fibers are unmyelinated and responsible for dull, throbbing, and persistent pain, typically associated with inflammation and infection.
When the pulp is inflamed, it releases inflammatory mediators like prostaglandins and cytokines. These chemicals sensitize the nerve endings, lowering their pain threshold and amplifying the pain signals. The confined space within the tooth's anatomy means that even a slight swelling of the pulp can lead to a significant increase in pressure, which further irritates these nerves. Interestingly, studies have shown that pain can be more severe in mandibular (lower jaw) teeth, which can be particularly challenging to anesthetize effectively.
Factors That Influence Your Pain Experience
Not everyone experiences endodontic pain in the same way. Several factors can influence how you perceive and react to discomfort:
- Pre-treatment Pain Levels: One of the strongest predictors of how much pain you might experience after a procedure is how much pain you were in beforehand. If you arrive at our office in severe pain, you might be more sensitive to any post-treatment discomfort.
- Genetics: Our genetic makeup can play a role in how we perceive and process pain. Some individuals naturally have a higher or lower pain threshold.
- Gender Differences: Research suggests there can be gender differences in pain perception, with some studies indicating that males may experience less severe endodontic pain than females.
- Psychological State and Dental Anxiety: Your mental state significantly impacts your pain experience. Anxiety and fear can heighten your perception of pain. We know that dental fear can develop early in life and can make any dental visit feel more daunting. Addressing these psychological factors is a crucial part of our patient-centered approach. For more insights into how psychological factors influence dental experiences, you can explore scientific research on dental fear.
Immediate At-Home Relief While Waiting for Your Appointment
Waiting for your endodontic appointment, especially when you're in pain, can feel like an eternity. While these home remedies are temporary fixes and not a substitute for professional treatment, they can offer significant endodontic pain relief and make you more comfortable until you can see us.

Simple Steps for Quick Comfort
Here are some non-pharmacological approaches you can try at home to manage your symptoms:
- Cold Compress: Apply a cold compress or an ice pack wrapped in a cloth to the outside of your cheek, near the affected area. Use it for 15 minutes on and 15 minutes off. This can help reduce swelling and numb the area, providing temporary relief.
- Head Elevation: When lying down or sleeping, try to keep your head liftd with extra pillows. This can help reduce blood flow and pressure in the affected area, potentially easing the throbbing sensation.
- Salt Water Rinses: Rinse your mouth with a warm saltwater solution. Dissolve one teaspoon of salt in a cup of warm water and swish it around your mouth for about 30 seconds before spitting it out. This helps to clean the area, reduce inflammation, and can soothe irritated tissues.
- Avoiding Trigger Foods: Steer clear of foods that might aggravate your tooth. This includes anything extremely hot or cold, as well as sugary or acidic items, which can increase sensitivity or irritate exposed nerves.
- Soft Diet: Stick to soft, lukewarm foods that require minimal chewing. This reduces pressure on the painful tooth.
Here's a list of safe, soft foods that can be gentle on your sensitive tooth:
- Yogurt
- Smoothies
- Pudding
- Mashed potatoes
- Cooked cereals (oatmeal, cream of wheat)
- Soft-cooked pasta
- Scrambled eggs
- Soups (lukewarm)
- Bananas
- Avocado
Traditional Remedies: What Works and What to Watch For
Sometimes, people turn to traditional remedies for toothaches. One of the most well-known is clove oil.
- Clove Oil (Eugenol): Clove oil contains eugenol, a natural antiseptic and anesthetic. It has been used for centuries to numb pain. To use it, apply a very small amount of clove oil directly to the affected tooth and surrounding gum using a cotton swab. Be cautious, as too much can irritate the gums. It offers temporary relief by numbing the nerve endings.
- Risks and Precautions: While clove oil can provide temporary relief, it's important to use it sparingly and ensure it doesn't get onto surrounding healthy tissues, as it can cause irritation. It's also not a cure and shouldn't delay professional treatment.
Other traditional remedies like peppermint tea bags (applied to the tooth) are sometimes mentioned for their soothing properties, but scientific evidence is limited. Always remember that these are stop-gap measures. The best path to lasting endodontic pain relief is through professional dental care.
Professional Endodontic Pain Relief Strategies
When you visit us for endodontic treatment, our priority is to ensure your comfort and provide effective endodontic pain relief. We use a combination of advanced techniques and compassionate care to make your experience as pleasant as possible.
Ensuring a Pain-Free Procedure
A key component of our approach is achieving profound local anesthesia. We understand that the thought of a dental procedure can be intimidating, but modern anesthetics and techniques allow us to numb the area thoroughly, so you feel little to no pain during your treatment.
- Local Anesthesia: We typically use local anesthetics like lidocaine or articaine to completely numb the tooth and surrounding tissues. For challenging cases, especially in the mandibular (lower jaw) teeth which can be notoriously difficult to anesthetize due to their dense bone structure, we employ advanced techniques. This includes the Inferior Alveolar Nerve Block (IANB), often supplemented with buccal infiltration of articaine or even intraligamentary injections. Studies show that premedication with anti-inflammatory drugs like diclofenac sodium and paracetamol before an IANB can significantly improve anesthetic success and reduce post-operative pain. We also use a "cold test" to confirm profound pulpal anesthesia, as a "numb lip" alone isn't always enough to guarantee a pain-free procedure.
- Sedation Options: For patients who experience dental anxiety, we offer various sedation options to help you relax. Nitrous oxide, commonly known as "laughing gas," can help ease your nerves and make the procedure more comfortable. We also offer oral sedatives for those who need a deeper level of relaxation. Your comfort is paramount to us, and we tailor our approach to your individual needs. More info about our approach to patient comfort
Clinical Techniques for Endodontic Pain Relief
Beyond anesthesia, we employ specific clinical techniques to manage and prevent pain, both during and between appointments:
- Occlusal Reduction: This involves carefully adjusting the biting surface of the affected tooth. If a tooth is inflamed and sensitive to pressure, reducing its contact with opposing teeth can significantly decrease post-treatment pain. Research indicates that occlusal reduction can lower the risk of moderate to severe pain by about 40% within 12 hours post-instrumentation, and the overall risk of pain by 25% within 24 hours.
- Incision and Drainage (I&D): For cases involving an abscess with fluctuant (palpable) swelling, an I&D procedure is performed. This involves making a small incision to drain the pus and relieve pressure, providing immediate and substantial endodontic pain relief. While mock I&D (without actual drainage) has shown some success due to psychological factors, actual drainage is crucial for infection resolution.
- Trephination: In some acute cases, where an abscess has not yet drained, trephination can be performed. This creates a small opening through the bone or tooth to allow for drainage of inflammatory exudate, rapidly relieving pressure and pain.
- Re-instrumentation: If pain persists between appointments, especially in non-vital teeth, re-instrumentation might be necessary. This involves re-cleaning and shaping the root canal system, along with thorough irrigation, to remove any residual microbial debris that could be causing the flare-up.
- Intracanal Medicaments: After initial cleaning, we may place intracanal medicaments inside the tooth to reduce bacteria and inflammation. Ledermix paste, a corticosteroid-antibiotic compound, has been shown to be particularly effective in reducing postoperative pain, especially in cases of pulpal necrosis and acute apical periodontitis. Corticosteroids themselves have a proven postoperative pain-reducing effect in endodontic patients.
Your Guide to Post-Treatment Pain Management
After your endodontic procedure, it's normal to experience some mild discomfort or soreness as your body begins the healing process. However, this post-procedure pain is typically much less intense and more manageable than the pain you felt before treatment. Our goal is to ensure your recovery is as smooth and comfortable as possible. We provide clear post-operative instructions and are always here to address any concerns. More info about emergency care
Pharmacological Approaches to Endodontic Pain Relief
We rely on a combination of medications to effectively manage any discomfort after your treatment.
| Medication Type | Mechanism of Action | Potential Side Effects |
|---|---|---|
| Ibuprofen (NSAID) | Acts peripherally to inhibit cyclooxygenase (COX), reducing prostaglandin synthesis, decreasing inflammation, fever, and pain. | Gastrointestinal upset (nausea, heartburn, abdominal pain), renal issues, increased risk of cardiovascular events. |
| Acetaminophen | Acts centrally to block pain signaling, likely by inhibiting prostaglandin synthesis in the central nervous system. | Liver toxicity (hepatotoxicity) if exceeding daily limits (4,000 mg/day). |
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Medications like ibuprofen and diclofenac are often our first line of defense. They work by reducing inflammation at the site of the pain. Prophylactic intraligamentary injection of diclofenac sodium has been shown to be more effective than oral administration in reducing postoperative pain.
- Combination Therapy: For superior endodontic pain relief, we often recommend a combination of ibuprofen and acetaminophen. These two medications work synergistically: ibuprofen tackles inflammation peripherally, while acetaminophen blocks pain signals centrally. This dual action is highly effective for mild to moderate pain, often outperforming opioids and with fewer side effects.
- Prescription Medications: In some cases, stronger non-narcotic options may be prescribed. For example, intranasal ketorolac has been shown to significantly reduce both preoperative and postoperative pain. A single oral dose of 10 mg ketorolac or 100 mg tapentadol administered before treatment can also significantly reduce postoperative pain. We prioritize nonnarcotic medications over opioids in almost all clinical situations due to the severe adverse effects and potential for abuse associated with opioids. We align with guidelines from the CDC and ADA, which emphasize maximizing nonpharmacologic and nonopioid pharmacologic therapies for dental pain. For further guidance on pain management strategies, refer to the CDC guidelines on dental pain care.
The Role of Antibiotics and When to Call Your Dentist
Antibiotics play a specific role in endodontic pain management, primarily when bacterial infection is present and spreading.
- Managing Infection: While antibiotics are not a primary pain reliever, they can help reduce pain by eliminating the bacterial source of infection, especially when NSAIDs are contraindicated or for patients with acute apical abscesses. Valacyclovir combined with amoxicillin, for instance, has shown a significant decrease in pain for patients with moderate-to-severe pain from acute apical abscesses. However, antibiotics are not routinely recommended for treating every endodontic flare-up; definitive root canal treatment and drainage are usually more effective.
- Antibiotic Overuse Concerns: We are mindful of the growing concern regarding antibiotic resistance. Therefore, we prescribe antibiotics judiciously, only when there's clear evidence of bacterial infection that warrants their use, and not for routine postoperative pain where non-opioid analgesics are sufficient.
- Signs of Persistent Infection or Complications: While most post-treatment discomfort resolves quickly, it's crucial to know when to contact us urgently. You should call your dentist immediately if you experience:
- Fever: A sign that your body is fighting a spreading infection.
- Excessive Swelling: Swelling that increases significantly or spreads to your face or neck.
- Unbearable Pain: Pain that intensifies or is not controlled by prescribed or over-the-counter medications.
- Pus or Drainage: Any signs of pus or drainage from the treated area or nearby gums.
- Persistent dental infection: If you suspect the infection is persisting or worsening.
These symptoms could indicate a post-treatment flare-up or a persistent infection that requires immediate attention. Your health and comfort are our top priorities!
The Future of Pain-Free Endodontics
The field of endodontics is constantly evolving, with researchers and clinicians always seeking new ways to improve endodontic pain relief and improve patient outcomes. We are excited about the cutting-edge therapies on the horizon that promise even more comfortable and predictable treatments.
Cutting-Edge Therapies on the Horizon
These emerging techniques are paving the way for truly pain-free endodontic experiences:
- Platelet-Rich Fibrin (PRF): PRF is a concentrated blood product derived from your own blood, rich in growth factors that promote healing. Studies suggest that PRF is superior to other materials in reducing pain in endodontic surgeries, accelerating tissue regeneration, and minimizing post-operative discomfort.
- Intracanal Cryotherapy: Imagine using cold to reduce pain! Intracanal cryotherapy involves irrigating the root canal with chilled saline solution (around 2.5 °C) as a final step. This significantly reduces postoperative pain compared to standard irrigation, offering an effective, economical, and safe method for pain management in single-visit root canal treatments.
- Low-Level Laser Therapy (LLLT): LLLT, also known as photobiomodulation, uses specific wavelengths of light to stimulate cellular function, reduce inflammation, and alleviate pain. While some studies are ongoing, preliminary findings suggest that LLLT can reduce postoperative pain after endodontic procedures, offering a viable non-pharmacological alternative.
- Acupuncture: This ancient Chinese practice is gaining recognition in modern dentistry. Preoperative acupuncture has shown more significant pain reduction compared to placebo in patients with symptomatic apical periodontitis. It's considered a safer option for managing postoperative pain compared to some medications and can be a valuable adjunct to local anesthesia.
- GABAergic Signaling: Researchers are exploring the role of GABA (gamma-aminobutyric acid), an inhibitory neurotransmitter, in dental pulp. The presence of functional GABA receptors in dental pulp suggests that drugs targeting this signaling pathway could offer novel approaches for managing endodontic pain in the future.
These advancements highlight a future where endodontic treatment is not only effective at saving teeth but also virtually free from discomfort, making your dental experience as stress-free as possible.
Frequently Asked Questions about Endodontic Pain
We often hear similar questions from our patients about endodontic pain. Here are some of the most common ones, along with our expert answers:
Is a root canal supposed to be painful?
The perception that root canals are inherently painful is largely outdated. Thanks to modern endodontic techniques, advanced local anesthetics, and sedation options, the procedure itself is typically no more uncomfortable than getting a filling. Our goal is to make the experience as pain-free as possible. The pain you experience before the root canal, due to infection or inflammation, is almost always far worse than any discomfort during or after the procedure. You might feel some pressure during the treatment, but sharp pain should not be present.
What is the best over-the-counter medicine for severe tooth pain?
For effective endodontic pain relief from severe tooth pain, a combination of ibuprofen (an NSAID) and acetaminophen is often recommended. Ibuprofen (e.g., Advil, Motrin) works as an anti-inflammatory, reducing swelling and pain at the source. Acetaminophen (e.g., Tylenol) acts centrally to block pain signals. When taken together, their different mechanisms of action provide superior pain control compared to either medication alone, often surpassing the effectiveness of opioids for dental pain. Always follow the dosage instructions on the package or as advised by your dentist.
How long does pain last after a root canal?
It's normal to experience some mild to moderate discomfort or soreness for a few days (typically 24-72 hours) after a root canal, especially when chewing. This is part of the natural healing process as the tissues around the treated tooth recover. The intensity and duration of this discomfort can vary depending on the severity of the initial infection, your individual pain threshold, and how well you follow post-operative instructions. If your pain intensifies after a few days, you develop a fever, notice excessive swelling, or the pain is not managed by medication, please contact our office immediately. These could be signs of a complication that requires our attention.
Your Path to a Comfortable Recovery
Experiencing endodontic pain can be disruptive and concerning, but as we've discussed, there are many effective strategies for endodontic pain relief available today. From immediate at-home remedies to advanced professional treatments and careful post-operative care, your comfort and well-being are always our top priority.
We encourage you to take an active role in your recovery by following our instructions, taking prescribed medications as directed, and not hesitating to reach out if you have any questions or concerns. At CWD Dental Group, serving the communities of Tallahassee, Havana, Quincy, Crawfordville, and Wakulla, Florida, our experienced team is dedicated to ensuring your comfort at every stage of treatment. We use the latest techniques for effective pain management, helping you achieve lasting relief and a healthy smile. Learn more about our endodontist services.
